PROTECT TEXAS HEALTHCARE
On March 7, 2024, the Texas Health and Human Services Commission (HHSC) announced its intention to award contracts for STAR (Medicaid) and Children’s Health Insurance Program (CHIP), the two programs that cover most low-income children, pregnant women and families.
Protect the healthcare of 1.8 million Texans who stand to lose their current health plan if the proposed contract awards are not cancelled. Act now to stop the largest disruption in Texas Medicaid history.
SAVE
QUALITY CARE
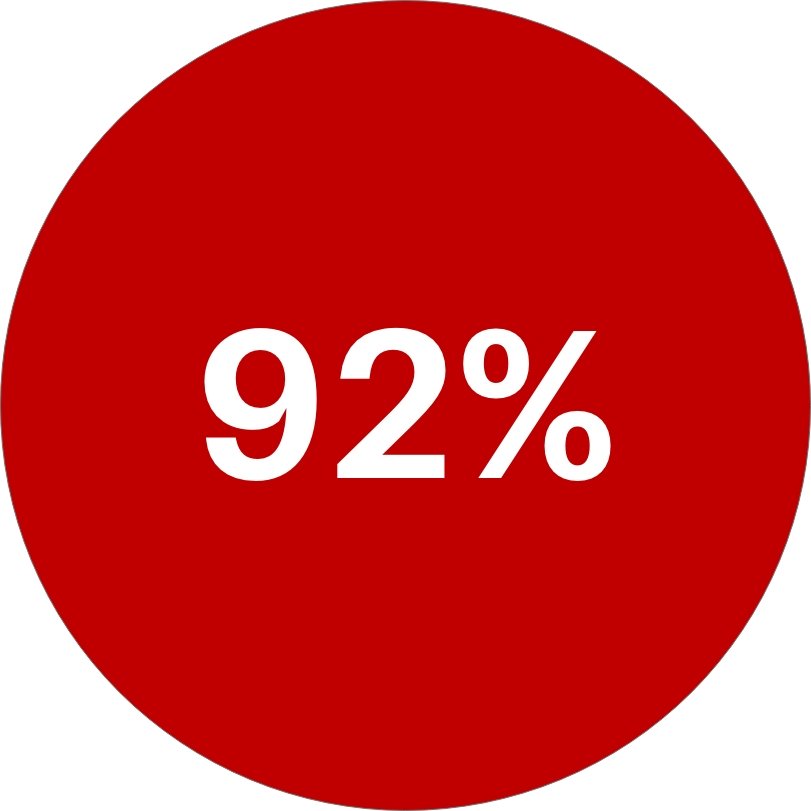
Prevent 92% of Texans from losing access to high-quality health plans.
PRESERVE
PLAN CHOICE
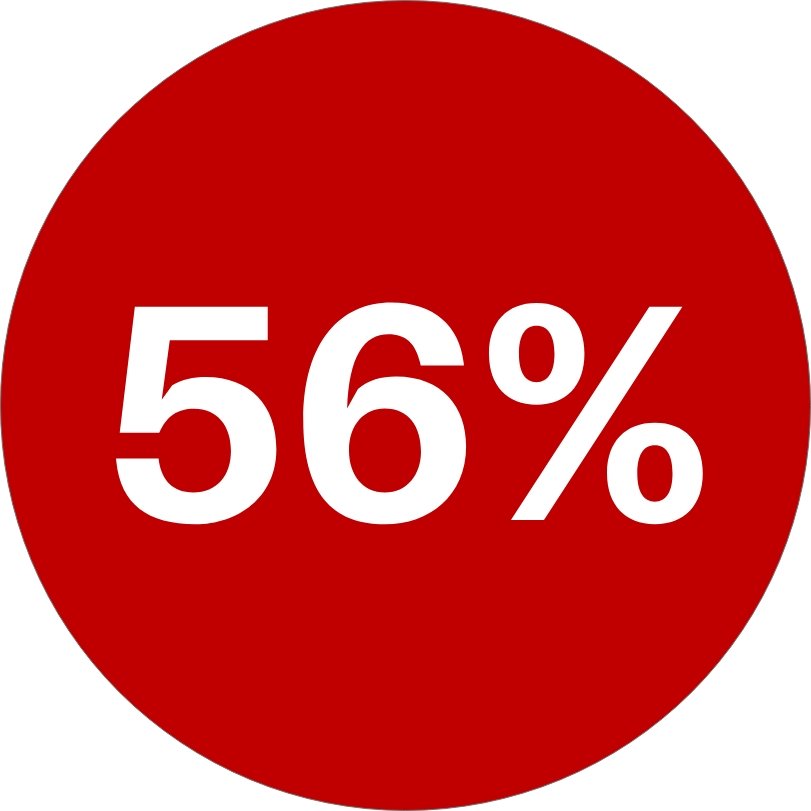
1.8M, or 56% of Texans,
will lose their
current health plan.
KEEP
CHILDREN’S HOSPITALS
Only 1 in 4 plans operated by children’s hospitals will receive contracts.
PROTECT
TEXAS JOBS
Prevent the $533M in lost wages that will result when 6,200 Texans lose their jobs.
SAVE QUALITY CARE
All Texans deserve access to quality care. HHSC’s decision reduces quality at the expense of the state’s families and children.
92% of the highest quality-rated health plans will be eliminated.
85% of members will have to choose a new - and potentially lower-performing - health plan.
PRESERVE HEALTH PLAN CHOICE
Nearly 2 million Medicaid members will lose their health plan, putting the health of children, pregnant women and families at risk.
56% will lose access to their current plan and could also lose access to their provider.
Only 1 in 4 children’s hospital health plans will receive contracts - drastically reducing care options for children.
PROTECT HIGH-PAYING JOBS AND THE TEXAS ECONOMY
If HHSC’s decision is not overturned, the impact on the Texas economy - including high-paying jobs, community investment and tax-based impact - will be significant.
$14.7 billion in lost healthcare services funds in the state.
6200 in lost jobs.
$533 million in lost wages.
PREVENT MORE PROCUREMENT FAILURES
The state has struggled with Medicaid procurements and this situation is no exception.
Six Medicaid contract awards or requests for proposal have been canceled due to scoring errors between 2015-2020.
Five commissioners over 10 years signals frequent leadership turnover and lack of oversight, enabling a track record of failed procurements.
A history of flawed contracting processes is outlined in multiple records, including the Strike Force Report.

TAKE ACTION NOW: TELL THE GOVERNOR TO CANCEL THE PROPOSED CONTRACT AWARDS
1.8 million children and families will lose their health plan, resulting in the largest disruption to member care in Texas.
High quality health plans will be removed, forcing individuals who rely on Medicaid to choose a new, lower quality plan and a new doctor.
The Texas economy will suffer, causing billions in lost healthcare services funds, along with millions in wages due to the potential loss of thousands of jobs.
The proposed contracts ignore what makes Medicaid work, including quality ratings, member choice and health plan provider networks.
By entering your information below, this letter will be sent to your state representative to tell the Governor to cancel the proposed Medicaid and CHIP contact awards.
KEY TERMS TO KNOW
MANAGED CARE: The term “managed care” describes a type of health care focused on helping reduce costs while keeping quality of care high. Managed care was introduced in Texas in 1993 and is now the primary mode of care for people who have Medicaid or CHIP coverage.
MANAGED CARE ORGANIZATIONS: Managed Care Organizations, or MCOs, are health insurers that contracts with the state to deliver Medicaid health benefits and additional services. These MCOs accept a set per member per month payment for these services. In Texas, there are currently 16 MCOs.
MEMBER CHOICE: Allowing members to choose their health plan is an integral part of managed care. In fact, 70% of members actively choose their plan instead of being automatically assigned to a health plan by the state.
STAR: Most people who have Medicaid in Texas get their coverage through the STAR program. STAR covers low-income children, pregnant women and families.
CHIP: The Children's Health Insurance Program (CHIP) covers children in families that earn too much money to qualify for Medicaid but cannot afford to buy private insurance.
SDA: A Service Delivery Area, or SDA, is a select group of counties, defined by HHSC, where different health insurance plans provide Medicaid and CHIP coverage. There are 13 SDAs in Texas.
RFP: A request for proposal, or RFP, is a business document that announces a project, describes it, and solicits bids from qualified contractors to complete it. Texas uses the RFP model for managed care organizations to bid and secure Medicaid and CHIP contracts.